Integrating Posture, Weight, Load, Spinal Degenerative Disease, Education of Postural Habits, and Chiropractic Care
The primary method of public transportation connecting the cities of the San Francisco Bay Area is a train system called BART (Bay Area Rapid Transit). BART passenger boarding platforms are often above ground adjacent to freeways. Driving by on the freeway, one can see dozens to hundreds of BART passengers waiting to board the next train; essentially all of them have their heads down and their necks bent forward while looking at their cell phones.
Reflecting on advances in technology over the past 120 years reminds us of how much technology has changed our lives. Automobiles, airplanes, space shuttles, drones, telephones, radio, television, computers, and so much more. This discussion will address cell phones.
The technology of cellular communications is important to everyone. Cellular technology is of particular importance to the chiropractic profession because cell phone use causes postural distortions. These postural distortions can have devastating effects on spinal joints, particularly the joints of the low neck (cervical spine) and upper back (thoracic spine). These spinal joint problems are collectively referred to as accelerated degenerative spinal joint disease or spondylosis (1, 2, 3, 4).
In addition, the prolonged postures associated with cell phone use are being linked to other health problems, including (5):
- Muscle fatigue and myofascial pain syndromes (muscle pain problems and headache) (6, 7, 8).
- Chronic muscle contraction that often results in headaches (9, 10).
Early on, cell phones had only one function: talking on the phone. Today, cellular devices are often referred to as smart phones because they engage in many other activities (5):
- Talking on the phone
- Texting
- GPS services
- Wi Fi services
- Entertainment: videos, games, surfing the web, Facetime, music, radio, podcasts, etc.
- News, traffic flows, banking, and other business applications.
Understanding the effects of chronic postural distortions from any cause requires basic knowledge of three key principles of biomechanics:
- viscoelastic creep
- weight v. load
- levers
Viscoelastic Creep
Biological systems adapt to prolonged mechanical loads. Tissues literally change in response to these loads; they adapt to become longer or shorter in response to the loads (11). This includes the biomechanical loads caused by the prolonged use of cellular devices. The technical term for this premise is called viscoelastic creep (12).
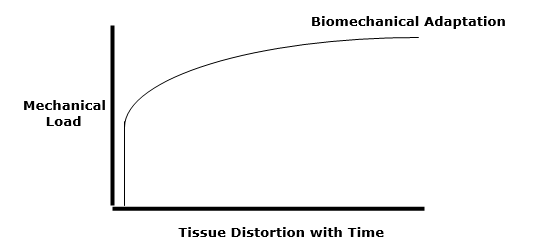
Soft tissues (ligaments, cartilage, tendons, muscles, etc.) undergo viscoelastic creep when prolonged loads are applied. The tissues mechanically distort and eventually adapt to the applied loads. This includes the tissue distortions caused by head-down posture and the forward bending of the cervical spine while viewing or working on hand-held cellular devices (13).
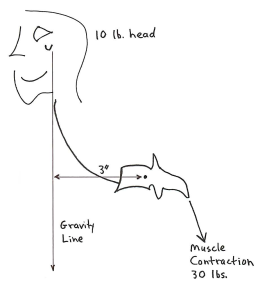
Weight is self-explanatory. For this discussion, assume that the head weighs 10 lbs. As explained by Katy Bowman in her 2017 book Move Your DNA: Restore Your Health Through Natural Movement, weight is far less important than is load (11). Load is weight multiplied by a lever arm:
“It’s not the weight that breaks you down, it’s the load created by the way you carry it.”
“Loads are often oversimplified to ‘weight’ because it makes them easier to understand, but there is much more going on with your sore knee (or foot, or back, or pelvic floor) than your weight.”
“Weight is not the be-all and end-all of loads. When you want to improve your health, it’s much more important to consider how you carry your weight than to spend hours contemplating the lone data point that is Your Weight.”
Levers
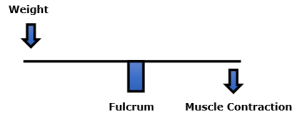
Upright posture is a 1st class lever mechanical system (12). The classic example of a 1st class lever mechanical system is a seesaw or teeter totter.
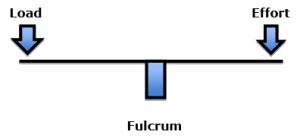
The fulcrum of a 1st class lever is the place where the forces are the greatest. These forces are dependent upon three factors:
- The weight of the object that is on one end of the lever
- The distance the weight is away from the fulcrum (lever arm)
- The addition of the counterbalancing effort required to remain balanced
Again, assume the head weighs 10 lbs. If the head’s weight is 10 lbs., and the distance (the lever arm) from the fulcrum was 10 inches, the load on the fulcrum would be 100 lbs. (10 X 10). In order to remain balanced, the effort on the opposite side of the fulcrum would have to also be 100 lbs. The effective load applied to the fulcrum would be 200 lbs. Thus, an actual load of 10 lbs. would have an effective load on the fulcrum of 200 lbs.
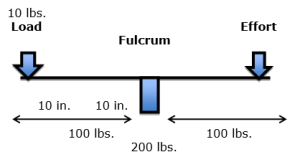
In the spine, the fulcrum of the 1st class lever of upright posture is the vertebral body/disc and the two facet joints. Pertaining to the head/neck complex, the load is the weight of the head multiplied by the distance between the center of mass of the head and the fulcrum (the vertebrae). The effort is the amount of force generated by the contracting muscles on the opposite side of the fulcrum to keep the system balanced.
Rene Cailliet, MD, nicely explains these concepts in his 1996 book Soft Tissue Pain and Disability (14). Dr. Cailliet notes that when a 10 lb. head is displaced forward with a 3-inch lever arm, the counter balancing muscle contraction on the opposite side of the fulcrum (the vertebrae) would have to increase by 30 lbs. (10 lbs. X 3 inches):
Recent Lay Articles
In 2017, Reuters Health published a study titled (15):
Leaning Forward During Phone Use May Cause 'Text Neck'
This article makes these points:
- Spine surgeons are noticing an increase in patients with neck and upper back pain, likely related to poor posture during prolonged smartphone use.
- Young patients who should not have back and neck issues are reporting disc hernias and spinal alignment problems.
- In an x-ray, the neck curve typically is being reversed as people look down at their phones for hours each day.
- Prolonged abnormal stresses on a growing spinal column may lead to abnormal spinal development with dire long-term spinal health consequences in adulthood.
- Simple lifestyle changes are suggested to relieve the stress from the “text neck” posture, including holding cell phones in front of the face while texting and using two hands and two thumbs to create a more symmetrical and comfortable position for the spine.
- People who work on computers or on tablets should use an elevated monitor stand that sits at a natural horizontal eye level.
- Take frequent rest breaks and/or engage in some physical exercise that can strengthen the neck and shoulder muscles.
••••
In 2018, The New York Post published a study titled (16):
Tech is Turning Millennials into a Generation of Hunchbacks
This article profiles the situation of a young man who began suffering from upper-back pain and neck soreness while in his late teens, subsequent to a habit of hunching over his cellular phone. As his symptoms progressed, he developed constant pain, he hunched his shoulders, and the pain caused him to wake up numerous times throughout every night.
After a decade of suffering, the patient’s chiropractor diagnosed him with “tech neck,” explaining that the cause was the forward/bent neck posture he assumed while using his laptop and iPhone. “Tech neck” is a painful forward head syndrome. It is an increasingly common condition caused by slumping over devices for hours a day, leading to a reversal of the natural neck spinal curve and triggering a physiological imbalance in the upper body.
The loss or reversal of the normal cervical curve is easily diagnosed with postural x-rays.
“Undoing the damage is a process that includes breaking bad habits, taking standing breaks and doing exercises such as yoga, foam rolling and stretches that promote good carriage and strengthen core and upper body muscles. Experts also advise patients to hold mobile devices with their elbows at 180 degrees so the screen is in front of their faces.”
Treatment options included chiropractic, restorative postural traction, and postural and core exercises.
Medical Literature Studies
In 2014, a study was published in the journal Surgical Technology International, titled (13):
Assessment of Stresses in the Cervical Spine
Caused by Posture and Position of the Head
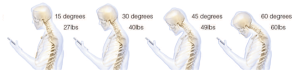
In this article, the author notes that billions of people are using cell phone devices, essentially in poor posture. The purpose of this study was to assess the forces incrementally seen by the neck (cervical spine) as the head is tilted forward, worsening forward head posture.
The author indicates that in 2014, the average person spent 2-4 hours a day with their heads tilted forward reading and texting on their smart phones, amassing 700-1400 hours of excess, abnormal cervical spine stress per year. A high school student may spend an extra 5,000 hours in poor posture per year.
The author notes:
“Poor posture invariably occurs with the head in a tilted forward position and the shoulders drooping forward in a rounded position.”
“The weight seen by the spine dramatically increases when flexing the head forward at varying degrees.”
“Loss of the natural curve of the cervical spine leads to incrementally increased stresses about the cervical spine. These stresses may lead to early wear, tear, degeneration, and possibly surgeries.”
••••
In 2017, a study was published in the journal Applied Ergonomics, titled (17):
Texting on Mobile Phones and
Musculoskeletal Disorders in Young Adults
The aim of this study was to examine whether texting on a mobile phone is a risk factor for musculoskeletal disorders in the neck and upper extremities in a population of young adults, aged 20-24 years. The study duration was 5 years.
The authors indicate that young adults have grown up with mobile phones as an ever-present part of their lives. Access to mobile phones was 99% in the group of young adults they studied. In the United States, text messaging is the most frequently used type of communicative medium.
The authors note that text messaging places a repetitive physical stress on the neck, shoulders, arms and thumbs. The authors concluded:
“Sitting with the head bent forward while texting was more common among those with musculoskeletal symptoms.”
“Associations were found between text messaging and reported pain in the neck/upper back, shoulder/upper extremities, and numbness/tingling in the hand/fingers for both men and women.”
“There were clear associations between the highest category of text messaging and pain in the neck/upper back.”
“Sustained neck flexion may be a risk factor for developing pain in the neck, shoulder, and upper extremities.”
“Sitting with the head bent forward without supporting the arms causes a static load in the neck and shoulder muscles, which could explain the reported pain from neck/upper back.”
“Sustained muscle load and posture are considered to be risk factors for developing musculoskeletal disorders.”
“Associations with neck and upper extremity pain were found at levels of text messaging as low as 6 texts/day.”
“The strongest associations with neck/upper back and shoulder pain concerned the highest exposure category (>20 texts/day) in both men and women.”
These authors believe that the associations between cell phone use and health symptoms are underestimated because they did not include data on how much the participants use their mobile phones for other activities, e.g. gaming.
••••
Also in 2017, a study was published in The Spine Journal, titled (18):
“Text Neck”
An Epidemic of the Modern Era of Cell Phones?
The authors note that cellular/smart phones are everywhere. They are being extensively used by people of all ages. A concern to the modern era physician is the potential musculoskeletal consequence of this extensive cell phone usage, especially texting.
Extensive cell phone use and associated postures cause spondylotic changes consistent with an aged spine, but they are now being found in younger and younger age groups, including:
- Disc herniations
- Kyphotic alignment
- Abnormal imaging studies
The authors suggest that the rise in the number of patients with neck and upper back pain is related to accelerated cervicothoracic disc degeneration. These authors propose that there are significant increases in intradiscal pressure during flexion, and that “chronic increased intradiscal pressure likely contributes to disk degeneration [cervical spondylosis] and herniation.”
These authors also cite a study of over 7,000 young adult subjects (age 20–24) over a 5-year period that showed “persistent neck pain and upper back pain is associated with time spent text messaging.”
“It now seems rather clear that repetitive texting, or similar activity while using a forward flexed neck position, may lead to neck pain or ‘text neck.’”
These authors have great concern for the consequences of prolonged cervical spine flexion while texting on the developing (growing) spine. They note that persistent, prolonged forward flexed neck position may lead to anterior ligamentous contractures, accelerating cervical disc degeneration and cervical kyphosis.
These authors make these recommendations to avoid and/or treat text/tech neck:
- Patients hold their cell phone up at or near eye level while texting.
- “For patients who spend significant time working at a computer or tablet we recommend the use of elevated stands for desktop monitors so that the monitor is at a natural horizontal gaze level.”
- Subjects should perform basic exercises that stretch and strengthen the cervical and upper thoracic soft tissue.
••••
In 2019, a study was published in the journal Current Reviews in Musculoskeletal Medicine, titled (19):
The Relationship Between Forward Head Posture and Neck Pain:
A Systematic Review and Meta-Analysis
The purpose of this study was to determine if forward head posture (FHP) is associated with neck pain. It is a systematic review and meta-analysis that used 15 cross-sectional studies that included 2,339 subjects. This is the first systematic review estimating the relationship between neck pain measures and FHP.
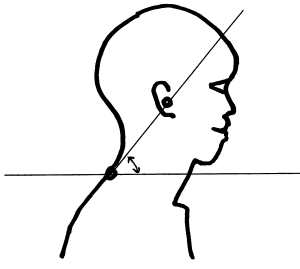
The craniovertebral angle is the measured angle between the horizon and a line from the tragus of the ear to the spinous process of C7. A decrease in this angle indicates a greater FHP, and it is considered an accurate measure to discriminate FHP severity. “The craniovertebral angle was a significant predictor for lifetime prevalence and doctor visits due to neck pain.”
The authors note that forward head posture (FHP) is the most common cervical postural fault in the sagittal plane and is found in almost all populations. Increased time texting on mobile phones or using computers may have a long-term impact on neck pain due to prolonged periods of neck flexion. The authors state:
“Maintaining a high flexion angle of the neck during work leads to an increase in the weight of the head which puts extra load on the spine and leads to changes in ligaments, tendons, and muscles which may progressively cause permanent changes of posture in the form of FHP.”
“There was a statistically significant difference in FHP between adults with neck pain and asymptomatic adults; i.e., adults with neck pain showed a greater FHP than asymptomatic adults.”
“The results showed that adults with neck pain show increased FHP when compared to asymptomatic adults and that FHP is significantly correlated with neck pain measures in adults and older adults.”
“Neck pain was significantly associated with holding the neck in a forward bent posture for a prolonged time.”
“The results showed that adults with neck pain have significantly more FHP than asymptomatic adults.”
••••
In 2021, a study was published in the International Journal of Environmental Research and Public Health, titled (20):
Text Neck Syndrome in Children and Adolescents
The authors present a case report of a 16-year-old female presenting with headache, dizziness, neck pain, vertigo, and ataxia. She had no fever or trauma. All labs were normal. Eye examination was negative. There was no vestibular pathology. MRI (Magnetic Resonance Imaging) of the cervical spine showed a reversal of cervical lordosis and posterior disc protrusion at the C4–C5 level. The doctor’s working diagnosis was “text neck syndrome.”
The authors note that the improper use of personal computers and cell phones might be related to the development of a complex cluster of clinical symptoms commonly defined as “text neck syndrome.” Children and adolescents spend 5 to 7 hours a day on their smartphones and handheld devices with their heads flexed forward to read and text. The cumulative effects of this exposure cause an alarming excess stress to the cervical spinal structures. The authors state:
The “text neck syndrome has increased stresses on the cervical spine, which can lead to cervical degeneration along with other developmental, medical, psychological, and social complications.”
“This clinical condition refers to the onset of cervical spinal degeneration that results from the repeated stress of frequent forward head flexion while we look down at the screens of mobile devices and while we text for long periods of time.”
“The weight of the head on the spine is dramatically increased when it is flexed forward, and the effects and amount of weight are strongly and progressively enhanced by varying the degrees.”
“Frequent forward flexion can change the cervical spine curvature, supporting ligaments, tendons, musculature, and the bony segments, commonly causing postural change and pain on the neck and associated areas.”
The authors make these “text neck” preventative recommendations:
- Keeping one’s spine in a neutral position as much as possible, avoiding excessive neck flexion.
- Avoid excessive device usage, and take frequent breaks.
- Position the device so that it reduces stress both on the head and neck.
- Limit the time of use of smartphones, tablets, and PCs.
••••••••••
Chiropractors are expertly trained in the ergonomic avoidance of the postures that lead to text/tech neck, advising and coaching thousands of patients on these issues daily. Chiropractic clinical practice offers a variety of treatment approaches that are very effective in the management of the text/tech neck syndrome (21, 22, 23, 24, 25, 26, 27, 28, 29, 30).
REFERENCES:
- Garstang SV, Stitik SP; Osteoarthritis; Epidemiology, Risk Factors, and Pathophysiology; American Journal of Physical Medicine and Rehabilitation; November 2006; Vol. 85; No. 11; pp. S2-S11.
- Ruch W; Atlas of Common Subluxations of the Human Spine and Pelvis, Second Edition; Life West Press; 2014.
- Uchida K, Nakajima H, Sato R, Yayama T, Mwaka ES, Kobayashi S, Baba H; Cervical Spondylotic Myelopathy Associated with Kyphosis or Sagittal Sigmoid Alignment: Outcome after Anterior or Posterior Decompression; Journal of Neurosurgery: Spine; November 2009; Vol. 11; pp. 521-528.
- Grosso M, Hwang R, Mroz T, Benzel, Steinmetz M; Relationship between degree of focal kyphosis correction and neurological outcomes for patients undergoing cervical deformity correction surgery; Journal of Neurosurgery: Spine; June 18, 2013; Vol. 18; No. 6; pp. 537-544.
- Davis D; Disconnect: The Truth About Cell Phone Radiation; 2013.
- Travell J, Simons D; Myofascial pain and dysfunction, the trigger point manual; New York; Williams & Wilkins; 1983.
- Travell J, Simons D; Myofascial pain and dysfunction, the trigger point manual: THE LOWER EXTREMITIES; New York; Williams & Wilkins; 1992.
- Simons D, Travell J; Travell & Simons’, Myofascial pain and dysfunction, the trigger point manual: Volume 1, Upper Half of Body; Baltimore; Williams & Wilkins; 1999.
- Seletz E; Headache of Extracranial Origin; California Medicine; November 1958; Vol. 89; No. 5; pp. 314-317.
- Bogduk N; Anatomy and Physiology of Headache; Biomedicine and Pharmacotherapy; 1995; Vol. 49; No. 10; pp. 435-445.
- Bowman K; Move Your DNA: Restore Your Health Through Natural Movement;
- White AA, Panjabi MM; Clinical Biomechanics of the Spine, Second Edition; Lippincott; 1990.
- Hansraj KK; Assessment of Stresses in the Cervical Spine Caused by Posture and Position of the Head; Surgical Technology International; November 2014; Vol. 25; pp. 277-279.
- Cailliet R; Soft Tissue Pain and Disability; 3rd Edition; FA Davis Company; 1996.
- Crist C; Leaning forward during phone use may cause 'text neck'; Reuters Health; April 14, 2017.
- Fleming K; Tech is Turning Millennials Into a Generation of Hunchbacks; The New York Post; March 5, 2018.
- Gustafsson E, Thoee S, Grimby-Ekman A, Hagberg M; Texting on Mobile Phones and Musculoskeletal Disorders in Young Adults: A Five-year Cohort Study; Applied Ergonomics; January 2017; Vol. 58; pp. 208-214.
- Cuéllar JM, Lanman TH; “Text Neck” An Epidemic of the Modern Era of Cell Phones?; The Spine Journal; June 2017; Vol. 17; No. 6; pp. 901–902.
- Mahmoud NF, Hassan KA, Abdelmajeed SF, Moustafa IM, Silva AG; The Relationship Between Forward Head Posture and Neck Pain: A Systematic Review and Meta-Analysis; Current Reviews in Musculoskeletal Medicine; December 2019; Vol. 12; No. 4; pp. 562-577.
- David D, Giannini C, Chiarelli F, Mohn A; Text Neck Syndrome in Children and Adolescents; International Journal of Environmental Research and Public Health; February 7, 2021; Vol. 18; No. 4.
- Leach RA; An evaluation of the effect of chiropractic manipulative therapy on hypolordosis of the cervical spine Journal of Manipulative and Physiological Therapeutics; March 1983; Vol. 66; No. 1; pp. 17-23.
- Harrison DD, Jackson BL, Troyanovich S, Robertson G, de George D, Barker WF; The efficacy of cervical extension-compression traction combined with diversified manipulation and drop table adjustments in the rehabilitation of cervical lordosis: a pilot study; Journal of Manipulative and Physiological Therapeutics; September 1994; Vol. 17; No. 7; pp. 454-64.
- Troyanovich SJ, Harrison DE, Harrison DD. Structural rehabilitation of the spine and posture: rationale for treatment beyond the resolution of symptoms; Journal of Manipulative and Physiological Therapeutics; January 1998; Vol. 21; No. 1; pp. 37-50.
- Harrison DE, Harrison, DD, Haas JW; CBP Structural Rehabilitation of the Cervical Spine; 2002.
- Harrison DE, Cailliet R, Harrison DD, Janik TJ, Holland B; A new 3-point bending traction method for restoring cervical lordosis and cervical manipulation: a nonrandomized clinical controlled trial; Archives of Physical Medicine and Rehabilitation; April 2002; Vol. 83; No. 4; pp. 447-w53.
- Morningstar MW, Strauchman MN, Weeks DA; Spinal manipulation and anterior headweighting for the correction of forward head posture and cervical hypolordosis: A pilot study; Journal of Chiropractic Medicine; Spring 2003; Vol. 2; No. 2; pp. 51-54.
- Harrison DE, Harrison DD, Betz JJ, Janik TJ, Holland B, Colloca CJ, Haas JW; Increasing the cervical lordosis with chiropractic biophysics seated combined extension-compression and transverse load cervical traction with cervical manipulation: nonrandomized clinical control trial; Journal of Manipulative and Physiological Therapeutics; March-April 2003; Vol. 26; No. 3; pp. 139-151.
- Ferrantelli JR, Harrison DE, Harrison DD, Stewart D. Conservative treatment of a patient with previously unresponsive whiplash-associated disorders using clinical biomechanics of posture rehabilitation methods; Journal of Manipulative and Physiological Therapeutics; March- April 2005; Vol. 28; No. 3; pp. e1-8.
- Oakley PA, Harrison DD, Harrison DE, Haas JW; Evidence-based protocol for structural rehabilitation of the spine and posture: review of clinical biomechanics of posture (CBP) publications. Journal of the Canadian Chiropractic Association; 2000.
- Chu EC; Preventing the Progression of Text Neck in a Young Man: A Case Report; Radiology Case Reports; January 18, 2022; Vol. 17; No. 3; pp. 978-982.
“Authored by Dan Murphy, D.C.. Published by ChiroTrust® – This publication is not meant to offer treatment advice or protocols. Cited material is not necessarily the opinion of the author or publisher.”



